Cornea transplants 3d printing human cells eyes science is revolutionizing the field of ophthalmology. Current corneal transplantation methods, while effective, often face limitations. Imagine a future where damaged corneas could be replaced with perfectly engineered, 3D-printed substitutes grown from patients’ own cells. This exciting prospect is fueled by advancements in bioprinting technology and tissue engineering, promising a new era of personalized eye care.
This exploration dives into the intricate process of creating these revolutionary corneal tissues, examining the bioinks, cell sources, and ethical considerations. From the historical context of corneal transplants to the latest breakthroughs in stem cell therapies, we’ll unpack the science behind this burgeoning field. We’ll also address the challenges, highlighting the importance of responsible innovation in this transformative area of medicine.
Introduction to Cornea Transplants
Cornea transplantation, a life-saving surgical procedure, addresses severe corneal damage, restoring vision and improving the quality of life for countless individuals. The cornea, the transparent front part of the eye, plays a crucial role in focusing light onto the retina. Damage to the cornea, whether from injury, disease, or inherited conditions, can lead to significant vision impairment, impacting daily activities and social interactions.
Corneal transplantation provides a solution for such cases, offering a pathway to improved visual acuity and independence.This procedure has a rich history, with early attempts dating back centuries. While early methods were rudimentary, the development of more precise surgical techniques and improved tissue preservation methods have transformed corneal transplantation into a safe and effective procedure. The procedure is now widely performed worldwide, with a strong emphasis on minimizing trauma and maximizing patient outcomes.
Current Methods and Procedures
Modern corneal transplantation utilizes various techniques tailored to the specific needs of each patient. The process involves careful evaluation of the affected cornea and the selection of the most suitable donor tissue. Donor corneas are typically obtained from deceased individuals who have consented to organ donation. Strict protocols and rigorous testing ensure the safety and suitability of the donor tissue.
Surgical techniques are meticulous, focusing on precise tissue placement and minimizing potential complications. Post-operative care, including the use of appropriate medications and regular follow-up appointments, is essential for successful outcomes.
Challenges and Limitations
Despite significant advancements, challenges persist in corneal transplantation. The risk of rejection, where the recipient’s immune system attacks the transplanted tissue, remains a concern. Immunosuppressant medications are used to mitigate this risk, but they can have side effects. The availability of suitable donor corneas is another significant limitation. The demand for donor corneas often exceeds the supply, leading to waiting lists and potential delays in receiving treatment.
The meticulous surgical nature of the procedure also requires specialized training and experience from the surgical team.
Comparison of Corneal Graft Types
| Graft Type | Description | Suitability | Advantages | Disadvantages |
|---|---|---|---|---|
| Penetrating Keratoplasty | Entire diseased cornea is replaced with a donor cornea. | Severe corneal opacities, significant stromal damage. | Effective for extensive damage. | Higher risk of complications, including astigmatism and wound healing problems. |
| Lamellar Keratoplasty | Only a portion of the cornea is replaced, sparing the healthy layers. | Specific corneal diseases, less extensive damage. | Preserves more of the patient’s own healthy corneal tissue. Reduced risk of complications. | Not suitable for all cases of corneal damage. |
Penetrating keratoplasty (PK) is the traditional method involving the replacement of the entire diseased cornea. Lamellar keratoplasty, a more sophisticated approach, focuses on replacing only the damaged layers of the cornea, while preserving the healthy parts. The selection of the appropriate graft type is crucial and depends on the extent of the corneal damage and the overall health of the patient.
3D Printing of Human Cells for Cornea Regeneration: Cornea Transplants 3d Printing Human Cells Eyes Science

D bioprinting offers a revolutionary approach to corneal tissue engineering. By precisely depositing bioinks containing living cells, researchers aim to create customized corneal substitutes, potentially eliminating the need for donor corneas and addressing the global shortage of corneal tissue. This innovative technique promises to significantly improve the lives of individuals with corneal diseases and injuries.The fundamental concept behind 3D bioprinting for corneal regeneration involves creating a three-dimensional scaffold using bioinks.
These bioinks, which are biocompatible materials, act as a template for cell growth and tissue formation. Living cells are incorporated into the bioink, and the 3D printer carefully layers the bioink to construct the desired corneal structure. The resulting 3D-printed constructs can then be cultured to encourage the growth of new corneal tissue, ultimately providing a viable alternative to traditional corneal transplantation.
Bioinks for Corneal Tissue Engineering
Bioinks play a crucial role in the 3D bioprinting process. They provide structural support for cell growth and mimic the natural extracellular matrix (ECM) of the cornea. The selection of bioinks is critical, as their properties significantly influence the success of the tissue regeneration process. Different bioinks possess varying biocompatibility, mechanical strength, and printability characteristics.
Cell Sources for Corneal Tissue Engineering
Various cell sources can be utilized in the bioprinting process. Stem cells, such as mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs), are attractive due to their self-renewal capacity and potential for differentiation into corneal cell types. Human corneal epithelial cells and endothelial cells, isolated from donor corneas or from healthy individuals, also represent viable sources.
The choice of cell source influences the characteristics of the printed tissue, affecting its functionality and potential for integration within the recipient’s eye.
Advantages and Disadvantages of Different Bioinks
| Bioink Type | Advantages | Disadvantages |
|---|---|---|
| Hydrogels (e.g., collagen, hyaluronic acid) | Excellent biocompatibility, biodegradability, and cell adhesion; can mimic the natural ECM of the cornea | Limited mechanical strength, potential for swelling, and challenging to print complex structures |
| Alginate | High printability, good biocompatibility, and relatively low cost | Lower mechanical strength compared to other bioinks, potential for cell encapsulation, and limited biodegradability |
| Polycaprolactone (PCL) | High mechanical strength, good printability, and relatively high biocompatibility | Lower biodegradability compared to hydrogels, and potentially slower cell growth rates |
Examples of 3D-Printed Corneal Constructs
Researchers have successfully developed various 3D-printed corneal constructs. Some examples include constructs mimicking the layered structure of the native cornea, which consist of an epithelial layer, stroma, and endothelial layer. These constructs have shown promise in animal models, demonstrating the potential for regeneration of corneal tissue and restoration of vision. Future research focuses on improving the complexity and functionality of these constructs to achieve optimal outcomes.
Amazing advancements in cornea transplants are happening, with scientists exploring 3D printing human cells for eye regeneration. This innovative approach could revolutionize vision care. Meanwhile, for those looking to experience the thrill of VR gaming, the release date and pricing of Superhot VR on Sony PlayStation 4 PS VR are a key consideration. This article has all the details.
Ultimately, these advancements in both VR gaming and eye science demonstrate a fascinating future of technological possibilities and medical breakthroughs.
Creating a 3D-Printed Cornea from Human Cells
The process of creating a 3D-printed cornea from human cells involves several key steps. First, human corneal cells are isolated and cultured to obtain sufficient quantities for bioprinting. Then, a bioink containing these cells is prepared. The 3D bioprinter precisely deposits layers of the bioink to create the desired corneal structure. Subsequently, the printed construct is cultured in a controlled environment to promote cell growth and tissue maturation.
Finally, the mature corneal tissue can be transplanted into the recipient’s eye.
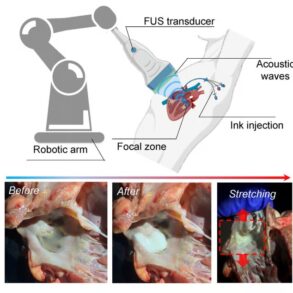
Integrating 3D Printing with Human Cells for Corneal Regeneration
The quest for corneal regeneration using advanced bioprinting techniques has emerged as a promising frontier in ophthalmology. This innovative approach aims to overcome the limitations of traditional corneal transplantation, offering a personalized and potentially more effective solution for restoring vision. The core principle involves utilizing 3D bioprinting to fabricate functional corneal tissue structures, mimicking the natural architecture of the cornea.This method leverages the precision of 3D printing to arrange living cells in a specific pattern, fostering their growth and organization into a viable tissue structure.
The key lies in the meticulous control over cell deposition and the careful selection of biomaterials, enabling the creation of a structure that mimics the mechanical and biochemical properties of a natural cornea.
Specific Steps in Creating Functional Corneal Tissue
Creating a functional corneal tissue using 3D printing and human cells is a multi-step process. It begins with the isolation and characterization of human corneal stromal cells. These cells are then cultured in a controlled environment to maintain their viability and proliferative capacity. Next, bioinks, biocompatible materials that encapsulate and support the cells, are carefully formulated. These inks are then precisely deposited layer by layer onto a bioprinter platform, following a pre-designed scaffold.
The bioprinting process meticulously arranges the cells within the scaffold, mimicking the intricate structure of a natural cornea. Finally, the printed construct is cultured in a specialized environment that promotes cell differentiation and tissue maturation, culminating in a functional corneal tissue ready for transplantation.
Crucial Factors Influencing Success
Several crucial factors determine the success of 3D-printed corneal tissue. The quality of the bioink, including its biocompatibility and ability to support cell growth, is paramount. The precise arrangement of cells within the 3D structure is also critical for optimal tissue formation. The specific type of cells used significantly impacts the final tissue’s characteristics. Furthermore, the culture conditions that promote cell differentiation and tissue maturation play a crucial role in achieving a fully functional cornea.
Adequate vascularization and nerve innervation are vital to the tissue’s long-term viability and function. Lastly, the post-printing culture environment must be carefully controlled to minimize any inflammatory response or tissue rejection.
Comparison with Other Tissue Engineering Methods
Compared to other tissue engineering methods, 3D bioprinting offers unparalleled precision and control over the arrangement of cells and biomaterials. While other techniques, like traditional cell culturing, may lack the ability to generate complex three-dimensional structures, bioprinting provides a highly controlled environment for tissue formation. Furthermore, the customization inherent in 3D bioprinting allows for the potential to create tissues tailored to the specific needs of individual patients, potentially reducing the risk of rejection and maximizing the therapeutic benefit.
Key Considerations for 3D-Printed Corneal Tissues, Cornea transplants 3d printing human cells eyes science
| Factor | Description | Importance |
|---|---|---|
| Cell Source | Type and quality of human corneal stromal cells | Directly affects tissue viability and function |
| Bioink Composition | Biocompatibility, biodegradability, and mechanical properties | Crucial for cell support and tissue structure |
| Printing Parameters | Resolution, deposition rate, and layer thickness | Impacts the fidelity of the 3D structure |
| Culture Conditions | Growth factors, nutrients, and oxygen levels | Essential for cell differentiation and tissue maturation |
| Post-Printing Evaluation | Assessing tissue structure, viability, and function | Critical for identifying potential issues and optimization |
Scientific Advances in Corneal Tissue Engineering
The quest to restore vision for those suffering from corneal damage is a driving force in regenerative medicine. Significant advancements in corneal tissue engineering, utilizing a multidisciplinary approach, offer promising avenues for treating corneal diseases and injuries. This field merges biological principles with engineering techniques to develop functional corneal substitutes.Recent research has focused on developing innovative strategies to regenerate corneal tissue, aiming to replace damaged or diseased tissue with functional substitutes.
This involves a combination of biomaterials, stem cells, and nanotechnology, all designed to create a supportive environment for corneal cell growth and regeneration. The progress in these areas promises to revolutionize the treatment of corneal diseases and improve the lives of countless individuals.
Stem Cell-Based Therapies
Stem cell therapies hold immense potential for corneal regeneration. The ability of stem cells to differentiate into various cell types, including corneal epithelial and stromal cells, makes them ideal candidates for tissue repair. Researchers are actively exploring different types of stem cells, including induced pluripotent stem cells (iPSCs) and mesenchymal stem cells (MSCs), for their potential in generating functional corneal tissue.
Studies are evaluating the effectiveness of these cells in restoring corneal transparency and function.
Nanotechnology in Corneal Tissue Engineering
Nanotechnology offers exciting opportunities to enhance the efficacy of corneal tissue engineering. Nanomaterials can be incorporated into bioengineered constructs to improve their biocompatibility, mechanical properties, and cellular interactions. The precise control over the size and shape of nanomaterials allows for tailored properties that can promote cell adhesion, proliferation, and differentiation.
Biomaterials for Corneal Regeneration
Biomaterials play a crucial role in creating scaffolds that support the growth and development of corneal cells. These scaffolds provide a three-dimensional framework for cells to adhere to and organize themselves into functional tissue. Different biomaterials, such as collagen, hyaluronic acid, and synthetic polymers, are being investigated for their suitability in corneal tissue engineering. Researchers are also exploring the use of natural biomaterials derived from the human body to ensure optimal biocompatibility and minimize the risk of rejection.
Current Research Directions
A key focus in current research is the development of bioreactors that mimic the natural corneal microenvironment. These bioreactors provide controlled conditions, such as temperature, oxygen tension, and nutrient supply, to optimize cell growth and differentiation. Furthermore, studies are investigating the integration of bioengineered corneal tissues with existing surgical techniques.
Ethical Considerations and Challenges
The burgeoning field of 3D-printed corneal tissues presents a fascinating blend of scientific advancement and complex ethical dilemmas. While the potential to restore sight for millions is undeniable, careful consideration of the ethical implications, safety concerns, and regulatory hurdles is paramount. This exploration delves into the nuanced challenges inherent in translating this technology into a widely accessible and safe clinical reality.
Recent advancements in cornea transplants, using 3D-printed human cells, are fascinating. Imagine the possibilities for restoring sight. This innovative technology is truly pushing the boundaries of science, and it’s a similar leap forward to something like the bmw 7 series remote parking assist , making complex tasks easier. This precision engineering, though, is still focused on the intricacy of the human eye and the hope of restoring vision.
Ethical Implications of 3D-Printed Corneal Tissues
The use of 3D-printed human cells for corneal transplantation raises profound ethical questions regarding the source of the cells, the potential for exploitation, and the equitable distribution of this potentially life-altering technology. Patient consent, informed decision-making, and the potential for coercion are critical considerations. Furthermore, the use of induced pluripotent stem cells (iPSCs) or other cell sources must be carefully evaluated in terms of their ethical implications, and the potential for unforeseen long-term consequences.
Safety Concerns Regarding 3D-Printed Corneal Tissues
Safety is paramount in any medical procedure. With 3D-printed corneal tissues, concerns arise regarding the potential for contamination during the printing process, the long-term biocompatibility of the printed material, and the potential for immune rejection. Stringent quality control measures are crucial to ensure the safety of the final product and minimize the risk of adverse reactions in recipients.
The risk of introducing unknown pathogens or cellular abnormalities through the printing process must be rigorously assessed and mitigated. The development and implementation of robust testing protocols are essential to establish the safety profile of these tissues before widespread clinical adoption.
Regulatory Frameworks for Corneal Tissue Engineering
Establishing clear and consistent regulatory frameworks is essential for ensuring the safe and ethical development and implementation of 3D-printed corneal tissues. This includes rigorous testing protocols for material compatibility, sterility, and long-term biocompatibility. Collaboration between regulatory agencies, researchers, and clinicians is crucial to create guidelines that address the unique challenges of this emerging technology. This collaboration must also include patient advocacy groups to ensure the voice of the potential recipients is heard.
Recent advancements in cornea transplants are fascinating, with 3D-printed human cells holding promise for restoring sight. It’s a remarkable leap forward in eye science. Speaking of impressive technology, I’ve been using my Google Pixel 7a for three months now, and it’s still a fantastic affordable pick. google pixel 7a 3 months later its still a great affordable pick The sheer potential of this technology to regenerate damaged tissues, like corneas, is genuinely inspiring and could revolutionize the field of eye care.
Challenges in Scaling Up Production of 3D-Printed Corneal Tissues
Scaling up the production of 3D-printed corneal tissues presents significant challenges. These include the cost-effectiveness of the process, the availability of skilled personnel, and the potential for variations in tissue quality across different production runs. Furthermore, the need for standardized manufacturing protocols and optimized bioprinting parameters is crucial for maintaining consistent tissue quality. The current manufacturing costs must be brought down to make the technology economically viable for large-scale deployment.
Potential Ethical Dilemmas and Proposed Solutions
| Ethical Dilemma | Proposed Solution |
|---|---|
| Unequal Access to Technology: High costs and limited availability of 3D-printed corneas could create disparities in access to care. | Implement financial assistance programs and explore public-private partnerships to reduce the cost of treatment and ensure equitable access. |
| Potential Exploitation of Cell Sources: Concerns regarding the ethical sourcing and use of cells for bioprinting. | Establish transparent and ethical guidelines for cell sourcing, ensuring fair compensation and appropriate oversight of cell banks. |
| Lack of Long-Term Safety Data: Uncertainty regarding the long-term effects of 3D-printed corneas. | Establish long-term follow-up studies to monitor the safety and efficacy of 3D-printed corneas and address potential long-term risks. |
| Informed Consent Issues: Ensuring patients fully understand the risks and benefits of 3D-printed cornea implants. | Develop comprehensive patient education programs, ensuring accessible and culturally appropriate information about the technology and potential risks. |
Future Directions and Implications
The potential of 3D-printed corneas extends far beyond immediate clinical application. This technology promises a transformative impact on healthcare, enabling personalized medicine and potentially revolutionizing how we approach eye care. The possibilities are vast, and the implications for patient outcomes and the future of ophthalmology are profound.The ability to create custom-designed corneal tissues tailored to individual patient needs holds immense promise.
This personalized approach could lead to improved outcomes, reduced complications, and potentially eliminate the need for donor corneas, significantly easing the burden on organ donation systems.
Potential Future Applications of 3D Printing in Corneal Transplantation
D printing technology can be leveraged to create a wide array of corneal structures beyond simple replacement. This includes creating intricate patterns for precise refractive correction, integrating drug delivery systems into the printed tissues, and even developing customized biocompatible materials. Such advancements would significantly enhance the precision and efficacy of corneal transplants. For instance, the possibility of incorporating growth factors directly into the 3D-printed scaffold could stimulate the regeneration of damaged corneal tissues, leading to accelerated healing and improved visual acuity.
Potential Impact of 3D-Printed Corneal Tissues on Healthcare Systems
The introduction of 3D-printed corneal tissues has the potential to significantly reshape healthcare systems. The reduction in reliance on donor corneas could alleviate the shortage of available tissues, which often limits the number of transplants performed annually. The standardization of 3D-printed corneal tissues could improve consistency in treatment and reduce variability in outcomes. This would result in a more predictable and reliable approach to corneal transplantation.
Further, reduced costs associated with the production of 3D-printed corneas compared to procuring donor tissues could make these treatments more accessible, particularly in underserved regions.
Future Research Directions in the Field of 3D-Printed Corneal Tissue Engineering
Future research should focus on refining the bioinks used for 3D printing, enhancing the biocompatibility and bioactivity of the materials, and optimizing the printing parameters to achieve higher resolution and more complex corneal structures. Investigations into the long-term stability and durability of 3D-printed corneas are crucial. The development of in-vitro models to assess the efficacy and safety of the printed tissues in a controlled environment is essential for the translation of this technology into clinical practice.
These research efforts will ensure that 3D-printed corneas are not only effective but also safe and reliable for long-term use.
Scenarios Where 3D-Printed Corneas Could Revolutionize Eye Care
Imagine a scenario where a patient with a severe corneal abrasion receives a customized, 3D-printed cornea designed to match their specific needs. The precise shape and thickness of the cornea could be optimized to correct refractive errors, potentially eliminating the need for subsequent laser eye surgery. Similarly, patients with inherited corneal diseases could benefit from personalized 3D-printed corneas that address the specific genetic defects, leading to more effective and targeted therapies.
Another scenario involves using 3D-printed corneas to create customized drug delivery systems for treating chronic eye conditions like glaucoma or keratitis.
Long-Term Implications of 3D Printing Technology for Corneal Transplantation
The long-term implications of 3D printing in corneal transplantation are far-reaching. Beyond improved patient outcomes, this technology has the potential to revolutionize ophthalmic procedures and foster new approaches to regenerative medicine. The potential for mass production of personalized corneal tissues could address the global shortage of donor corneas, making this life-saving procedure more accessible worldwide. Further, it could enable the development of new therapies and solutions for a broader range of eye diseases.
Closure

The prospect of 3D-printed corneas holds immense promise for restoring vision and improving the lives of countless individuals. While significant hurdles remain in terms of scalability and regulatory approval, the scientific advancements and ethical considerations are driving progress. This innovative approach to corneal regeneration is not just a scientific leap but a potential paradigm shift in eye care, paving the way for personalized and effective treatments.